This post may contain affiliate links. Please read our disclosure policy.
I wrote this post several years ago. Since then, I’ve heard from many parents who found themselves in a similar situation since then. Like me, these parents didn’t realize that a sleep disorder (or sleep deprivation) could be to blame for ADHD symptoms or misbehavior.
Parents who, like me, have seen their child return to the happy, patient, kind, joyful, well-behaved self. I wanted to share this again today in the hopes that it continues to help parents who are looking for the answer.
“I just don’t know what to do anymore,” I told my husband over the phone. He is just not himself anymore – he is getting upset about little things, he is grumpy all the time, and his behavior is just… off. He is misbehaving more & more. I don’t know what to do to help him.”
Little did we know at the time that our son’s sleep disorder was being disguised as ADHD or a behavior problem.
A Sleep Disorder May Be Misdiagnosed as ADHD
Let me start at the beginning before diving right into ADHD and sleep apnea…
E is our youngest son, and he was the BEST baby. He slept all night long (which was something I was NOT used to!) He never woke, not even in the middle of the night. 😉 He was happy all of the time.
Fast forward a few years. Our fourth child was born and that was also the exact same day that we learned that our son, E, had Hand, Foot & Mouth disease. It was so bad that his fingernails & toenails came off.
In fact, I had to stay in the hospital to keep his baby sister away for a few extra days. (sorry- a lot of information there, but wanted to include that because I often think it is what brought his issues to light).
Over the next few months, E started waking more often. I had not changed his bedtime routine at all, yet he was not able to stay asleep at night. He was also falling asleep extremely fast at night when it was time for bed, at 7:00.
The excessive daytime sleepiness (well, evening sleepiness) should have been a clue, but we attributed it to his Hand, Foot & Mouth and just assumed that he was having a hard time getting back to his normal sleep schedule.
Fast forward about five years… he was still waking at night. Still coming into our room every night (around the same time). Still tired in the mornings (and so grumpy when he woke up.)
That wasn’t all. His attitude and overall demeanor changed.
E had gone from a happy baby to a very unhappy, unpredictable, grumpy, hot-tempered child. He was now VERY quick to lose his temper, quick to get angry, and then quick to feel embarrassed when he realized that he had acted that way.
His behavior issues were growing.
E was that child that family members joked about as being a “hot head”. He was the one that made us timid to go out anywhere just in case he had a meltdown.
I knew, in my heart, that there had to be a reason that wasn’t just ‘misbehavior’. I knew, from his remorse, that he didn’t like acting this way and I was determined to help him.
Why was he acting this way? What on earth had we done differently? Nothing. We had raised them the same, yet he reacted to things in a completely different way than his older siblings.
I tried everything & nothing changed his behavior:
- no dyes,
- gluten-free diet,
- no processed foods,
- more outside time,
- special vitamins,
- massage therapy,
- more quiet time together talking through what we could do,
- problem-solving strategies,
- earlier bedtimes,
- etc…
Nothing worked. Even when I had hopes that I saw a difference, it wouldn’t last more than a couple of days.
Someone suggested that maybe he had ADHD or a behavior disorder.
I thought about it and thought that maybe he was showing symptoms of ADHD.
I knew that I could handle whatever was thrown at us, but I had to know WHAT we were dealing with, instead of just guessing. I had to know how to help him.
Finally, when I didn’t know what else to do – I took him to see a therapist. (Note: I am a Child Development Therapist and I had still no idea what to do with him because everything that “normally” worked with my clients wasn’t working with him).
So… we started therapy. I asked “Does my child have ADHD? I don’t know what else it could be?”
I went on to explain our past during our very first visit to a therapist. Immediately, she suggested seeing a neurologist to rule out any issues.
She suspected that the Hand, Foot & Mouth were to blame. I had always wondered about it, as well, so I called that day and made an appointment.
That started us on a very long journey to find out the truth.
After many appointments and questions like:
- Does he seem to have symptoms of attention deficit hyperactivity disorder?
- Does he seem to have restless legs at night (leaning towards restless legs syndrome)?
- Does he have high blood pressure or any learning disabilities?
When we went over his history and talked about any risk factors, the doctor ordered a sleep study.
Then the day came when our doctor called us in for an appointment to discuss the results.
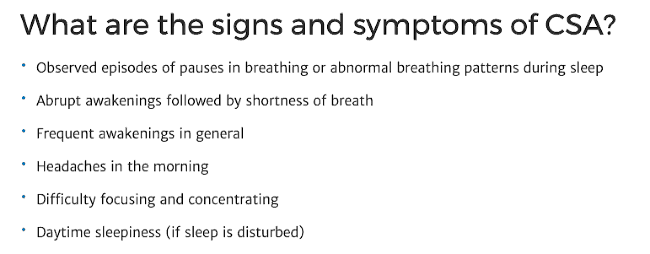
Our son had Central Sleep Apnea, “CSA”, and it was presenting as ADHD because of how it was changing his attitude and behavior.
“Central sleep apnea (CSA) is a pause in breathing during sleep, usually without snoring or gasping. Everyone experiences central apneas occasionally. However, if it occurs too frequently or for long periods of time, it can cause a decrease in the oxygen levels in the body and disrupt sleep.” ~Children’s Colorado.org
This was not SLEEP apnea as we knew it. It was not a blockage. It was not the same as obstructive sleep apnea. This was CENTRAL sleep apnea, caused by his brain telling him that he was drowning, pretty much, and making him get out of his REM sleep to ‘wake up and take a breath’.
This type of sleep apnea is often related to congestive heart failure and puts our son at a higher risk for breathing problems related to a heart condition.
So they sent him for more tests to rule out any of these further complications.
He did not have a heart condition or restless leg syndrome (also known as RLS.) Now we needed to fix his breathing patterns to help him so he sleeps through the night, every night.
What the doctor told us next explained the grumpiness, moodiness, temper tantrums, etc… in 11 little words:
“He is waking up 8 times every hour, all night long.”
Oftentimes, one of these wake-ups would lead to a 1-2 hour time of being awake. This is why the symptoms of sleep apnea often resemble the symptoms of ADHD. They are tired, grumpy, moody, and anxious due to lack of sleep.
A child waking at night is not rested enough to think or act the way that a rested child would think or act, and this is why they show that ADHD misdiagnosed is happening more & more.
ADHD Symptoms are Similar to symptoms of Sleep Deprivation
“Many ADHD symptoms are similar to symptoms of sleep deprivation. Among others, adult ADHD sleep problems include forgetfulness and difficulty concentrating. In children, fatigue may present as being hyperactive and impulsive8. Sometimes it can be difficult to tell whether these issues are brought on by ADHD or by a lack of sleep.
This may lead to misdiagnoses or may allow sleep disorders to go undetected. Experts, therefore, recommend screening patients for sleep problems before prescribing medication for ADHD.” – Sleep Foundation
Our poor sweet baby boy was barely sleeping.
Can you imagine how cranky that would make you? He was chronically tired, so by the time bedtime rolled around, he was exhausted and fell asleep within minutes.

We started looking into solutions for his sleep disorder.
He had many tests done because oftentimes, central sleep apnea is linked to a heart problem. Everything else came back normal and now we just had to help him. We started him on a CPAP machine to help him which took months to get right, but once we did, he was back. Our sweet, happy, selfless, caring E was back.
That was three years ago, and to say that his life changed is an understatement. He went from being the child that was unpredictable to being a child that you could rely on. He went from being the child that you hated to disappoint, because you knew how we would react, to being a child who could take things with a grain of salt.
Don’t get me wrong… he still had to unlearn the behaviors that he was used to (five years of “losing it” about things can change the way you handle things), but now he had the sleep that he needed and he could react in a calm way.
He is a different child.
He is himself again.
I soon found out that I wasn’t the only parent facing this…
Last week, I was online and read a Facebook post written by another mother… and that post went viral. It was like I had written it myself… Her name was Melody Yazdani and she was another mother of four.
Melody says in her post “Please share this” because her desire to help other mothers is so great. I reached out to Melody to let her know that I was writing this post and I couldn’t agree more. If only others knew that sleep disorders just don’t look like we think they do… hopefully this post will get the message out there.
“Parents, prepare yourself for some all caps yelling because this is going to change some lives…
All parents. If you have a child, I’m going to tell you something you need to know that you have probably never heard. And please share this.
There is a huge red flag in the picture I am sharing with this story. Do you see it?
CHILDREN SHOULD NOT BREATHE THROUGH THEIR MOUTHS. Not while awake, not while asleep. Never.
Symptoms that your child may have a sleep disorder:
If your child…
- falls asleep immediately after their head hits the pillow,
- snores,
- grinds their teeth,
- wakes up in the night,
- has night time accidents or daytime accidents,
- has impulse control issues,
- is hard to understand when speaking,
- has under-eye circles,
- has crooked teeth or a misaligned bite,
- wakes up insanely early,
- is irritable during the day,
- has a bad appetite,
Let me back it up to last year: My son, Kian, now age 8, determined, intelligent, feisty, and extremely active. He started school, no problems in Kindergarten. First grade rolled around, and we started getting behavior reports. “Kian pushed so and so” “Kian is having a hard time controlling his body”
Parent-teacher conferences, new reward system in place, and it seems to improve. But at home, it did anything but. When Kian gets angry, he gets ANGRY.
He gets fixated on little things (there is a hair in the shower, it’s gross! I can’t shower in there! *meltdown commences*), his fuse gets shorter and shorter, and he’s a picky eater who barely eats.
Second grade rolls around, and oh boy. While other kids are outgrowing their tantrums, Kian’s intensify and turn into daily spectacles, triggered by the smallest thing.
The behavior reports from school start rolling in. “Kian is pushing” “Kian can’t control his impulses” “Kian is having a hard time staying in his seat” and it going on and on. Almost daily. And I’m mortified.
Every morning it’s tantrum after tantrum before we even get out of bed.
Hitting, and throwing things, and the screaming. All the screaming. Starting at 5AM every morning.
We were at a loss – how did he become this way, what could be have done differently?
Kian starts seeing a therapist, recommended by his pediatrician. The therapist starts working with him and eventually recommends ADHD testing. Meanwhile, in the background, Kian has a persistent cough that just won’t go away, so we are also seeing a pulmonologist, and, against the advice of the pulmonologist, an allergist.
This will become relevant in a moment. Each doctor is recommending more and more medications – 2 inhalers for the cough, an antibiotic (4 different rounds) for the postnasal drip, a steroid, and it goes on and on. The therapist is dancing around ADHD, pushing us in that direction.
At a cleaning, Kian’s dentist makes an offhand comment about his teeth – they were ground almost halfway down, he’s grinding his teeth at night.
And then lightning struck, right at the perfect time. I stumbled upon an article that changed our life. The article, I’ve included at the bottom of the post, was about the connection between ADHD, sleep-disordered breathing, and mouth breathing. Every word in this article sounded like Kian.
This led me down a rabbit hole of research (the majority of which was done right in our back yard at the National Institute of Health) where I learned the following: Mouth breathing is NOT NORMAL and has long-term consequences for health.
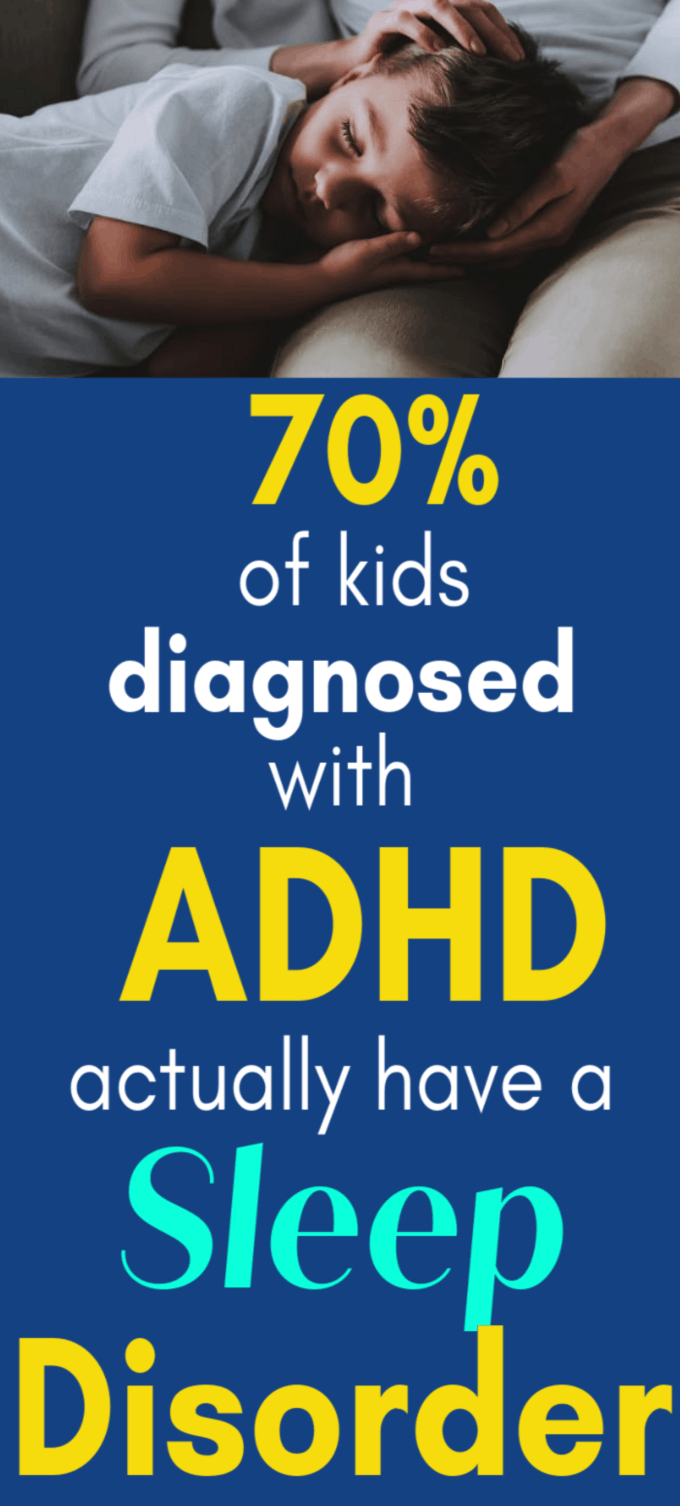
Sleep deprivation in children and ADHD exhibit the same symptoms.
The EXACT SAME SYMPTOMS.
⇒ Studies have been done (see NIH studies & references at the bottom of the post) where they took medicated ADHD kids, fixed the sleep-disordered breathing, and within 6 months 70% of the children had seen a resolution in symptoms and were no longer medicated.
As in, their ‘ADHD’ was cured. Because it wasn’t ADHD.
In 70% of children. Let that sink in.
This means that 70% of those children had been misdiagnosed with ADHD when they actually had a treatable sleep disorder.
Stimulants – Of course, they work, until they don’t. If you are sleep deprived, taking a stimulant will, of course, help you focus and feel ‘normal.’ But the brain is never fully resting – and hence the side effects
- nervousness,
- agitation,
- anxiety,
- sleep problems (insomnia),
- stomach pain,
- loss of appetite,
- weight loss,
- nausea,
- suicidal ideation’
Imagine yourself with, let’s say, three days of sleep deprivation. How? Multiply that times 100.
Now throw a stimulant in the mix.
How do you think you’ll feel once you start coming down from that?
The list goes on and on (I have copied some of the research links below).
Our story has a happy ending.
After a visit to an ENT and a sleep study, he was diagnosed with sleep apnea and sinusitis. He got exactly 0 minutes of REM sleep during the first study, and oxygen saturation in the low 80%, and his sinuses were 90% blocked.
We had no idea that Kian had a headache daily, but it was just his normal so he never thought to tell us. Kian had his tonsils and adenoids removed and the change was immediate.
He could breathe through his nose as he came out of surgery, where he couldn’t when they wheeled him in.
We have seen a complete 180 in behavior.
No more angry tantrums, no more fixation on little OCD things, it’s been an enormous change. And we haven’t even finished the second step – fixing his jaw and tongue issues that developed during the course of undiagnosed sleep apnea.
Our followup sleep study?
360 minutes of REM sleep, and oxygen saturation above the minimum threshold. No behavior reports in school. His appetite has exploded, he’s no longer a picky eater, and he had a huge growth spurt 2 weeks after the surgery.
He still has mild sleep apnea, but the frequency in the night was cut in half, and the duration of each episode was cut in half. If we see this much of a change now, I can only imagine how much it will improve once we cross the finish line.
Here’s why I am sharing:
No one, in my 12 years of parenting, ever told me any of this.
All the signs were there, right in front of our eyes, and I had no clue.
Kian’s pediatrician, who we loved and trusted, never said a word. The therapist had no clue, the pulmonologist, the allergist, even the ENT and sleep doctor didn’t believe me when I insisted he is seen for this invisible health issue. Not during any of our regular appointments, or during any of our sick child appointments.
And not until we have tangible proof with sleep study results and sinus imaging did anyone believe. I had to find this, diagnose this, and push for treatment myself. And thank God I did.
If any of this is raising red flags in your mind, if this sounds like your child, if your child has been diagnosed with ADHD, please see an ENT and get a sleep study. It may just change your life.
Please share this, you may help someone – I wish I had learned this information years ago!” – Melody, Facebook Post
(She also writes that while she is grateful for the reach of her post, she can not help to diagnose any children, but that she made an appointment directly, without a referral. We did the same.) ♥♥♥
How common is ADHD misdiagnosed?
Often. According to the Centers for Disease Control and Prevention, ADHD is the most commonly diagnosed behavioral disorder for kids in the United States, with at least 4.5 million diagnoses among children under age 18.
Can ADHD be mistaken for anxiety?
Yes. According to Child Mind Institue, ADDitudeMag, “Common symptoms occur for a variety of reasons and can reflect several different diagnoses. That’s why a good mental health professional will give your child a thorough evaluation based on a broad range of information before coming up with a diagnosis. It’s crucial to understand what’s really behind a given behavior because, just as in medicine, the diagnosis your child receives can drastically change the appropriate treatment.
ADHD medications, for example, won’t work if a child’s inattention or disruptive behavior is caused by anxiety, not ADHD.
According to Additude Mag, “Anxiety Disorders (AD) occur much more frequently in people with ADHD than they do in the general population. … ADHD and anxiety disorder symptoms overlap. Both cause restlessness. An anxious child can be highly distracted because he is thinking about his anxiety or his obsessions.”
Can ADHD be misdiagnosed as Dyslexia?
Unfortunately, Yes. “Sometimes people confuse ADHD with dyslexia, but they are different disabilities. Learning Disabilities is a language-based learning disability; ADHD is a deficiency of attention. When you treat ADHD, the symptoms of dyslexia may improve; the new-found capability for paying attention helps in reading.” – Additude Mag
Dr. Russell Barkley, author of Taking Charge of ADHD: The Complete Authoritative Guide for Parents, Suggests that children with ADHD are more likely to have a learning disability, like dyslexia. According to The Very Well Mind, they both show the same symptoms of poor penmanship, trouble with fluency, and distraction.
So what can you do?
According to Sleep Review Magazine: “Dentist Michael Fulbright, DDS, sleep apnea in children is a big problem, particularly when it goes undiagnosed or is misdiagnosed entirely. “These days, many children are being diagnosed with ADHD (attention deficit hyperactivity disorder). Some of them are acting out in school and getting in trouble. Well-meaning doctors may misdiagnose some of these children and prescribe Ritalin for ADHD, when really the cause of their behavioral problems may be sleep apnea,” he says in a release.
I highly suggest being 100% sure that your child has ADHD before starting any medication. Have the doctors do a sleep study to be on the safe side. I wish we had done ours years ago.
Take care & good luck! You are your child’s voice… their advocate & their support.
We only have a few years to really be present (and we can make the true difference in their lives when we spend these years wisely.)
I want to invite you to sign up for my FREE e-mail series called One on One time. It is completely free & I will send you this calendar to get you started. 🙂
More Posts You Might Like:
– Is your child waking too early? Try this.
– Mommy, will you lay with me?
.
..


*REFERENCES:
https://www.washingtonpost.com/…/could-adhd-be-a-type-of-s…/
https://scholar.google.com/scholar…
https://scholar.google.com/scholar…
https://www.sciencedirect.com/…/artic…/pii/S1087079213001329
https://www.medpagetoday.com/primarycare/sleepdisorders/2984
https://pediatrics.aappublications.org/content/129/4/e857…
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4261322/
https://www.ncbi.nlm.nih.gov/pubmed/17584620
https://www.ncbi.nlm.nih.gov/pubmed/17157069
https://www.ncbi.nlm.nih.gov/pubmed/15339263
https://www.ncbi.nlm.nih.gov/pubmed/12612236
https://www.ncbi.nlm.nih.gov/pubmed/21599769
https://www.ncbi.nlm.nih.gov/pubmed/22425033
https://www.ncbi.nlm.nih.gov/pubmed/25563906
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295456/
https://www.journal-imab-bg.org/…/JofIMAB-2018-24-1p1878-18…
https://www.jaypeejournals.com/eJournals/ShowText.aspx…







Hi, Becky. Thank you for writing this post, many things about it are sounding like our 3rd child. I was wondering if you have explored any natural solutions such as oils.
Oils can not fix sleep apnea. If you have this question, you may need to read to understand what sleep apnea is and the long and short term consequences of it for adults and children.
Thank you for sharing your story. We went through a very similar situation as Kian with our 4yo son. Had a b
Very persistent caugh and very angry, hot head, impulsive behavior. Was diagnosed with SPD. I realized something was reallly wrong with his sleeping when we went on vacation and he slept in my bed. Then it still took months of trying to figure out what was wrong with doctors. After he had his tonsils and adenoids out he was a completely different child. Parents, doctors and therapists all need to be aware of this condition.
When you had regular doctor appointments, at any time were their oxygenated blood levels low?
No.
I’m literally crying while reading this. My son has been diagnosed with ADHD. And while he does have some of the classic symptoms, lack of focus, irritability, etc. I have also complained for YEARS about his sleep problems.. Which the dr’s say is caused by is ADHD. Yet the sleep problems have not gone away even after putting him on medication for ADHD. His teacher always mentions how tired he seems in class, he’s 10 but goes to bed at 8pm every night and falls asleep right away. He wakes frequently throughout the night, grinds his teeth, occasionally snores, and upon waking, complains of headaches and that his “heart hurts”. The Dr has been dismissive chalking it up to anxiety. Thanks to your article I no longer feel crazy and will be insisting on an appoitnment with an ENT and requesting a sleep study.
Could you share a link to the NIH article with the 70% figure? I’d love to read it and share with my husband! (He’s applying to medical school and it would be a great thing to keep in mind.)
The article mentioned above:
https://www.washingtonpost.com/…/could-adhd-be-a-type-of-s…/
And if you want the research behind it, this is the tip of the iceberg (there is more):
https://scholar.google.com/scholar…
https://scholar.google.com/scholar…
https://www.sciencedirect.com/…/artic…/pii/S1087079213001329
https://www.medpagetoday.com/primarycare/sleepdisorders/2984
http://pediatrics.aappublications.org/content/129/4/e857…
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4261322/
https://www.ncbi.nlm.nih.gov/pubmed/17584620
https://www.ncbi.nlm.nih.gov/pubmed/17157069
https://www.ncbi.nlm.nih.gov/pubmed/15339263
https://www.ncbi.nlm.nih.gov/pubmed/12612236
https://www.ncbi.nlm.nih.gov/pubmed/21599769
https://www.ncbi.nlm.nih.gov/pubmed/22425033
https://www.ncbi.nlm.nih.gov/pubmed/25563906
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295456/
https://www.journal-imab-bg.org/…/JofIMAB-2018-24-1p1878-18…
http://www.jaypeejournals.com/eJournals/ShowText.aspx…
https://digitalscholarship.unlv.edu/cgi/viewcontent.cgi…
Is there a link to the NIH study you can provide? Thank you!
The article mentioned above:
https://www.washingtonpost.com/…/could-adhd-be-a-type-of-s…/
And if you want the research behind it, this is the tip of the iceberg (there is more):
https://scholar.google.com/scholar…
https://scholar.google.com/scholar…
https://www.sciencedirect.com/…/artic…/pii/S1087079213001329
https://www.medpagetoday.com/primarycare/sleepdisorders/2984
http://pediatrics.aappublications.org/content/129/4/e857…
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4261322/
https://www.ncbi.nlm.nih.gov/pubmed/17584620
https://www.ncbi.nlm.nih.gov/pubmed/17157069
https://www.ncbi.nlm.nih.gov/pubmed/15339263
https://www.ncbi.nlm.nih.gov/pubmed/12612236
https://www.ncbi.nlm.nih.gov/pubmed/21599769
https://www.ncbi.nlm.nih.gov/pubmed/22425033
https://www.ncbi.nlm.nih.gov/pubmed/25563906
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295456/
https://www.journal-imab-bg.org/…/JofIMAB-2018-24-1p1878-18…
http://www.jaypeejournals.com/eJournals/ShowText.aspx…
https://digitalscholarship.unlv.edu/cgi/viewcontent.cgi…
My kindergartner couldn’t wait to get back to school after a 3 week international trip, but it has been hell ever since – like he never re-adjusted. We’ve explored OT for sensory issues and he has mostly been able to self regulate, but he has been impossible ever since our trip – the school is baffled. We are baffled. We have wondered about sleep because he grinds his teeth and comes into our room at the same time every night and is super grumpy and tired despite 11-12 hours of sleep. We have a psych exam coming up. I know he has a sinus obstruction, just mouth breathing and no snoring. His behavioral issues the last couple months are coming between me and my husband and i can’t work (I can’t go too far from school because I have to respond daily), and it’s obviously impacting his confidence- lots of negative self talk. Heartbreaking. These stories sound so familiar that I just called to schedule a sleep study. Thank you for sharing.
Can you supply a link to the NIH article please ?
The article mentioned above:
https://www.washingtonpost.com/…/could-adhd-be-a-type-of-s…/
And if you want the research behind it, this is the tip of the iceberg (there is more):
https://scholar.google.com/scholar…
https://scholar.google.com/scholar…
https://www.sciencedirect.com/…/artic…/pii/S1087079213001329
https://www.medpagetoday.com/primarycare/sleepdisorders/2984
http://pediatrics.aappublications.org/content/129/4/e857…
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4261322/
https://www.ncbi.nlm.nih.gov/pubmed/17584620
https://www.ncbi.nlm.nih.gov/pubmed/17157069
https://www.ncbi.nlm.nih.gov/pubmed/15339263
https://www.ncbi.nlm.nih.gov/pubmed/12612236
https://www.ncbi.nlm.nih.gov/pubmed/21599769
https://www.ncbi.nlm.nih.gov/pubmed/22425033
https://www.ncbi.nlm.nih.gov/pubmed/25563906
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295456/
https://www.journal-imab-bg.org/…/JofIMAB-2018-24-1p1878-18…
http://www.jaypeejournals.com/eJournals/ShowText.aspx…
https://digitalscholarship.unlv.edu/cgi/viewcontent.cgi…
Hi! How can I contact you directly. Have same symptoms with your story, and he is 5 already- soon school, so I’m worried!
if no addenoids found, still surgery needed? We went to sleep check up, no epilepsy signs or Braindamage. To meet a good doctor over here is thing of pure luck, never know. Mother from Tallinn.
I’m not sure, because our son has central sleep apnea, which is very different from normal sleep apnea. (Our son’s central sleep apnea is not related to a blockage or anything with is mouth or throat).
Sorry- I wish that I had more advice to offer.
That’s wonderful that you found a solution and figured it out. How wonderful that he’s doing better. As you noted, this is way more common than we think. Did you know many of these symptoms and diagnosed conditions are listed as adverse events on vaccine inserts? Was your son vaccinated?
Thank you so much for your his article. It’s like someone visited my brain from the inside and written out all my emotions and exited feels. It all started when my son diagnosed with severed egg allergies at 6 months old and he is now 2.5y/o. I’m still working at his sleeping disorder and refused to believe that he has ADHD and is a misbehaving child. He is a determined, sweet, caring and clever little guy.
Did you have any issues getting them to treat the central sleep apnea? My son (who also has epilepsy) had a sleep study and they saw mild central apnea, but said they don’t treat it in children. At a neuro-psych eval earlier in the summer they saw attention deficits. As I’ve researched, I definitely think the impulse control and hyperactivity he displays is more related to his sleep. Even mild sleep apnea seems like it would build up night after night. Any advice on how to proceed?
He was put on a CPAP machine, but that’s it. It’s hard because it is controlled by the brain, whereas regular sleep apnea is more of a physical issue. (Turns out that CSA is very rare).
The machine worked very well. He wakes 3 times an hour now, but that is a HUGE improvement over 8 times an hour.
Hi Becky, this is so enlightening! Three years on, does your son still use the CPAP machine? Is Central Sleep Apnea something a child grows out of? You’ve inspired us to take the plunge to have our child observed at a sleep clinic.
Yes, he does. We took a break because he was doing so much better & the doctor gave us permission, but his mood began to change, so we went back to using it again. The ONLY issue is that it did push his jaw back slightly (the pressure of the mask on their tiny faces all night long can move the jaw ever-so-slightly, which can move the position of their teeth a bit) and we had to see an orthodontist and he now has a spacer & he will need braces. With that being said, it made such a difference for him that I’d never second guess it.
Wow! This hits SO close to home! Our daughter is 7 and at 2.5, got hand, foot, and mouth, and her great sleeping habits flew out the window!! For the last 4+ years, we have tried everything in the book to help her sleep, and I recently started exploring ADHD symptoms because we just can’t get to the bottom of it, but part of me really doesn’t think that is it. We did have a sleep study done, and she was diagnosed with mild sleep apnea. Our ENT said he would remove tonsils and adenoids, but we also are dealing with some anxiety issues that affect her sleep, so I am hesitant to jump into surgery since it is mild, and I am concerned that recovery will cause even more anxiety. What are your thoughts based on your experience with your child? I know you aren’t a doctor, but just as a mom that has gone through something SO similar, I would love to hear your thoughts.
Hi, this sounds like my daughter. She is nine and struggle with her attention and sleep and so cranky all the time. How and what questions she I say to her doctor? How would I go about getting her been seen? Thanks
I would track her sleep for a week or so and take that to the doctor. I’d call a pediatric neurologist and go over all of the symptoms. It’s amazing how much difference we’ve seen since learning what was going on with him.